
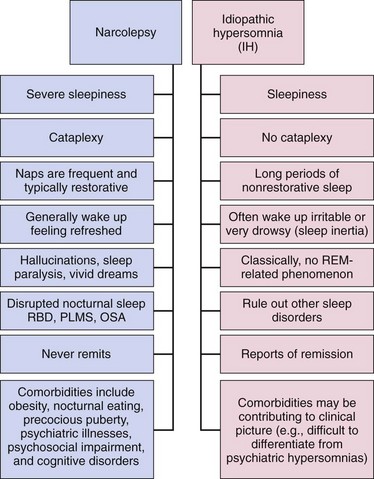
In a broader classification, diagnosing narcolepsy does not require cataplexy if REM sleep abnormalities (i.e., sleep onset REM sleep periods during multiple sleep latency test ) are objectively documented. Additionally, startling stimuli, stress, physical fatigue, or sleepiness may also be important triggers or factors that exacerbate cataplexy. Positive emotions such as laughter can more commonly trigger cataplexy than negative emotions, but any strong emotion is a potential trigger. Cataplectic events usually last from a few seconds to 2 or 3 minutes, but occasionally continues longer, however, the patient is usually alert and oriented during the event despite their inability to respond. Reduced muscle tone may be minimal, occurring in a few muscle groups and causing minimal symptoms (such as bilateral ptosis, head drooping, slurred speech or dropping things from the hand) or it may be so severe that total body paralysis occurs, resulting in complete collapse. Narcolepsy may therefore consist of an inability to maintain wakefulness combined with the intrusion of REM sleep associated phenomena (hallucinations, sleep paralysis and possibly cataplexy) into wakefulness.Ĭataplexy is the partial or complete loss of bilateral muscle tone in response to a strong emotion. Narcoleptic subjects feel refreshed after a short nap, but this does not usually last long and they become sleepy again within a few hours. The EDS of narcolepsy (as in other sleep disorders) can also cause related symptoms, including poor memory, reduced concentration, and irritability. These so-called "sleep attacks" are not instantaneous lapses into sleep, as is often thought by the general public, but represents the episodes of profound sleepiness experience by those with marked sleep deprivation. Additionally, irresistible or overwhelming urges to sleep occur from time to time during wakeful periods, commonly in untreated patients with narcolepsy. The EDS of narcolepsy presents itself with an increased propensity to fall asleep, nod, or easily doze in relaxed or sedentary situations, or a need to exert extra effort to avoid sleeping in these situations. Sleepiness or excessive daytime sleepiness (EDS) Cataplexy occasionally occurs in conjunction with other neurological conditions, such as Nieman-Pick Type C disease, but the pathophysiological links in these neurological conditions with the hypocretin abnormalities are presently not well established. Occurrence of cataplexy is tightly associated with impairment of hypocretin/orexin neurotransmission, and it rarely occurs as an isolated symptom. Although EDS is not specific for narcolepsy and is seen in other primary and secondary EDS disorders (such as sleep apnea syndrome), cataplexy is generally regarded as pathognomonic. Quality of life studies suggest that the impact of narcolepsy is equivalent to that of Parkinson's disease. Symptoms most often begin between adolescence and young adulthood, however it may also occur earlier in childhood or not until the third or fourth decade of life. Narcolepsy usually occurs in association with cataplexy and other symptoms, which commonly include hypnagogic or hypnopompic hallucinations, sleep paralysis, automatic behavior, and disrupted nocturnal sleep. 3.2 HLA, immune system, and etiology of narcolepsy.3.1 Deficiency in hypocretin (orexin) transmission in narcolepsy.2.3 Histocompatibility Human Leukocyte Antigen (HLA) testing.2.2 Cerebrospinal fluid (CSF) hypocretin-1 assessment.2.1 Polysomnography, nocturnal and daytime sleep studies.1.3 Hypnagogic or hypnopompic hallucinations.1.1 Sleepiness or excessive daytime sleepiness (EDS).


 0 kommentar(er)
0 kommentar(er)
